MEDICINE CASE DISCUSSION
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
I’ve been given this case to solve in an attempt to understand the topic of “patient
clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
CASE DISCUSSION
- fever since 5 days
- vomiting and pain abdomen since 3 days
history of present illness:
- patient was apparently asymptomatic 5days back she had high grade fever which was intermittent and not associated with chills and rigors
- 3days back and developed per abdominal pain and vomiting
- pain type: colicky type
- and she had an 2-3 episodes of vomiting per day which was non-projectile and non-bile stained
- generalized weakness and decrease appetite since 3 days
history of past illness:
treatment history:
personal history:
familial history:
physical examination:
Pallor: no
Icterus: no
Cyanosis: no
Lymphadenopathy: no
Edema: no
Clubbing of fingers: no
systemic examination:
CVS: S1 & S2 heard
no murmurs and cardiac thrills
ABDOMEN:
Inspection
the shape of the abdomen: scaphoid
palpation;
Tenderness- present in right hypochondrium, epigastrium, umbilical
no palpable mass
hernial orifices: normal
liver and spleen not palpable
percussion :
liver span: normal
auscultation;
bowel sounds: yes
CNS: intact
gait-normal
investigations
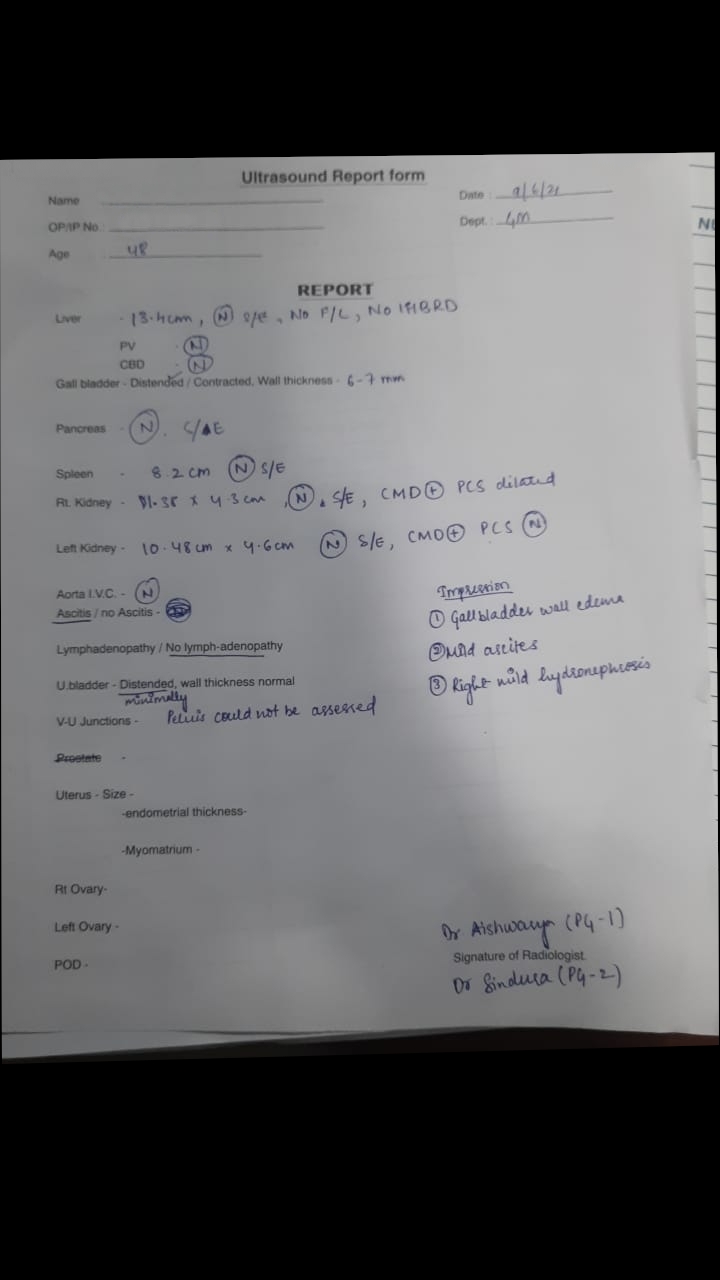
USG abdomen:
blood urea:
probable diagnosis:
treatment:
- i.v fluids: normal saline or ringer lactate at rate of 150ml/hr
- TAB.PAN 40MG OD in morning before breakfast
- INJ. OPTINUERON 1ampule in 100ml NS IV/OD
- TAB.DOLO 650MG BD
- BP/PR/TEMP/SPO2 monitoring every 4hours
- W/F bleeding manifestation









Comments
Post a Comment