A case of 45yrs old male with pitting type of edema
ROHITH SOMANI
MBBS 8th semester
roll no:127
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
I’ve been given this case to solve in an attempt to understand the topic of “patient
clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
CASE DISCUSSION
A 45yrs old male patient came with chief complaint :
-Swelling in lower limb since 4 months
-SOB since 4months
HISTORY OF PRESENT ILLNESS:
patient was apparently asymptomatic 4 months back and developed swelling over lower limbs which was insidious in onset
and gradually progressive.
More swelling was noticed in early morning
and reduces gradually
-SOB was sudden in onset and non progressive in nature .Aggrevated on walking and reduced on sitting or lying down.
PAST HISTORY:
no history of similar complaint in past.
Patient is a known case of Hypertension since 5yrs which increased from past 3 yrs
Patient is not know case of:DM,T.B,Asthma, Epilepsy
Patient has history of COVID-19 4 months back with chief complaint of cough and fever which was treated .
After 20 days of COVID-19 recovery he had pedal edema
TREATMENT HISTORY:
Anti- hypertensive drugs since 5years
LASIX since 4months
PERSONAL HISTORY:
Appetite- normal
Sleep - adequate
Bowel and bladder- regular
Diet - mixed
Toddy - consumption from age of 16 yrs and stopped consuming 4 months back
FAMILIAL HISTORY:
No history of similar complaint in family members
GENERAL EXAMINATION:
Pallor- yes
Icterus- no
Cyanosis - no
Clubbing- no
Lymphadenopathy- no
Edema- yes
vitals:
temperature:98.4 degree Fahrenheit
RR:20/min
PR:84/min
BP:140/100mm Hg
Spo2:98%
SYSTEMIC EXAMINATION:
CVS: S1 & S2 heard
no murmurs and cardiac thrills
RESPIRATORT SYSTEM:
dyspnoea - no
wheeze - no
position of trachea is central
Crepitus - not present
ABDOMEN:
Inspection
the shape of the abdomen: scaphoid
palpation;
Tenderness- not present
- no abnormal mass is palpable
Bowel sounds: not heard
liver and spleen not palpable
CENTRAL NERVOUS SYSTEM:
consciousness- conscious
Speech- normal
Neck stiffness-no
Kerning sign -no
Giat- normal
Sensory and motor system- intact
INVESTIGATION:
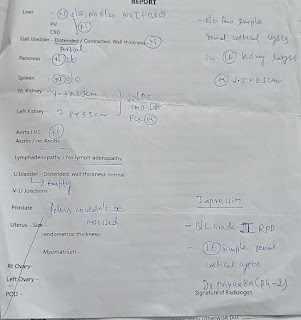
USG:
Serum creatinine:










Comments
Post a Comment