65yrs old male with complaints of burning micturition,low grade fever, bloating of abdomen,sob since 10days
65yrs old male with complaints of burning micturition,low grade fever, bloating of abdomen since 10days
ROHITH SOMANI
Roll no.147
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
I’ve been given this case to solve in an attempt to understand the topic of “patient
clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
CASE DISCUSSION:
Patient came to casualty with c/o low grade fever,burning micturition,bloating of abdomen since 10days
Patient c/o decreased appetite,sob since 10days
HOPI:
Patient was apparently asymptomatic 10days back then he developed low grade with chills, intermittent in nature, temporarily relieved on medication associated with burning micturition since 10days
C/o burning
micturition,urgency,hesitancy,dribbing, of urine and decreased stream.
C/o bloating sensation, belching,since 10days
C/o productive cough since 10days
SOB since 10days
Decreased appetite since 10 days
No c/o vomiting,loose stools,chest pain,orthopnoea,PND,pedal edema
Also informed that he hasn't passed stools since 4days
Daily chores
Patient is Sheppard by occupation daily he wake up around 6AM and goes to washroom ,will have a cup of tea and goes to farm come back around 10AM and will consume rice with curry around 12PM will take sheeps for feeding he will consume toddy around 1000ml return to home around 6PM and will have dinner(rice with curry) goes to sleep around 8PM
Since 15days he developed weakness,fever with chills,10days back .c/o of burning micturition went to local doctor and took medication ,symptoms got subsidised and then he stopped taking medication symptoms has reappeared
Past history
Diagnosed with DM2 10 days back
Not k/c/o HTN,CVA,CAD,TB,Asthma,thyroid disorder
PERSONAL HISTORY
Appetite decreased since 10days
Diet-mixed
Bowel and bladder - constipation and burning micturition since 10 days
H/o toddy consumption since 20 to 30 yrs
No history of allergy to food or drugs
GENERAL EXAMINATION
Patient is conscious, coherent, coperative. Moderately built moderately nourished
No pallor,icterus ,cyanosis, clubbing, generalised lymphadenopathy, generalised edema.
Vitals:
temperature:102F
Pulse rate: 82bpm
Resp rate:16cpm
BP:130/70mmhg
Spo2:98%
SYSTEMIC EXAMINATION
CVS
S1S2 heard
No cardiac murmurs
Apex beat heard at 5th ICS
Respiratory system
Normal vesicular breath sounds heard
Position of trachea - central
Abdomen
Inspection: shape-scaphoid
Umbilicus - central and inverted
No visible scars,engorged veins
All abdominal quadrants moving equally on inspiration and expiration.
Palpation: tenderness present in epigastric region
Liver and spleen not palpable
Percussion: resonant note heard all over abdomen on percussion
Auscultation: bowel sounds are not clearly heard on auscultation
CNS
Conscious,coherent and cooperative
Speech- normal
No signs of meningeal irritation.
Cranial nerves- intact
Sensory system- normal
Motor system:
Tone- normal
Power- bilaterally 3/5
Reflexes: Right. Left.
Biceps. ++. ++
Triceps. ++. ++
Supinator ++. ++
Knee. ++. ++
Ankle ++. ++
Investigations 30/7/23
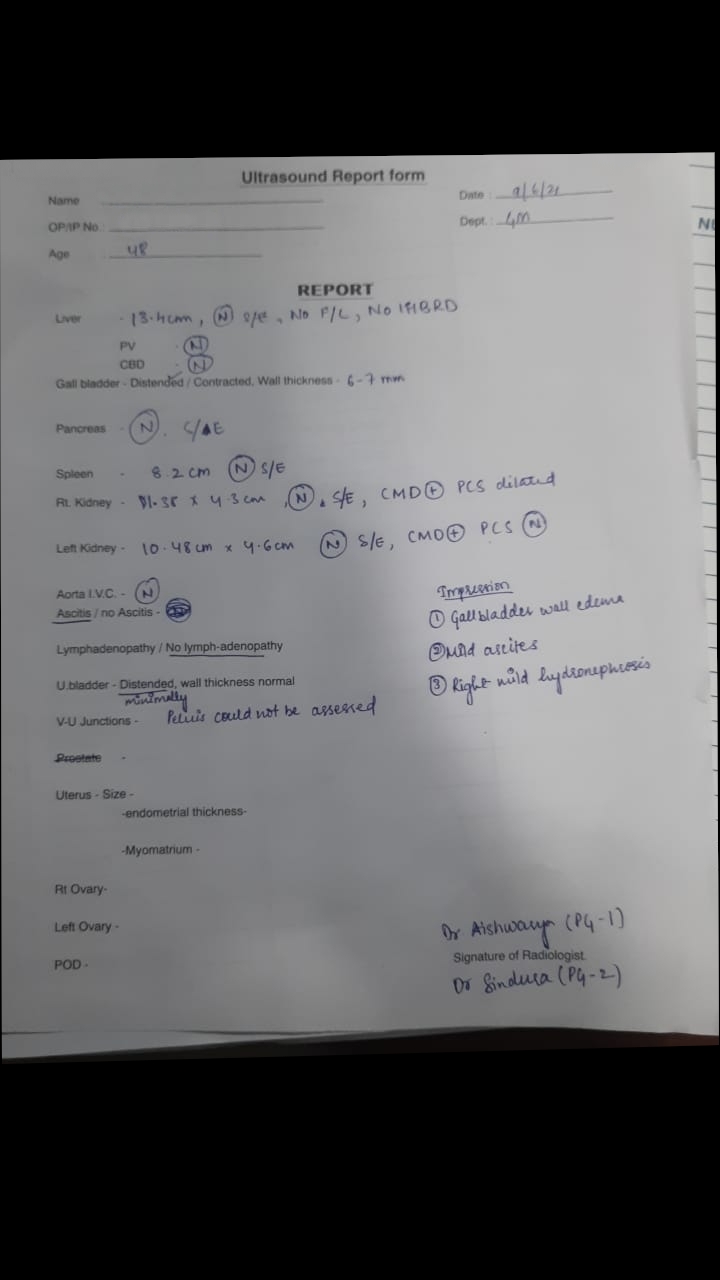
USG abdomen-
1)Left complex renal cortical cyst(20x19mm)
2)right simple renal cortical cyst(10x10mm)
3)B/L grade 1 RPD changes noted
USG chest
1)Right mild pleural effusion with underlying lung collapse with consolidectomy changes noted
2)left mild pleural effusion with consolidectomy change noted
BGT-O positive
RBS-121mg/dl
FBS-119mg/dl
Hemogram
Hb-9
TLC-18,500
Neutrophil-85
Lymphocytes -7
PCV-25.2
MCHC-35.7
RBC-3.27
Platelet-2.66
RFT on 30/7/23
Urea-78
Creatine - 1.9
Na+ -134
K+ - 3
Cl- 98
LFT
Total bilirubin -0.79
Direct bilirubin -0.19
SGOT-80
SGPT-63
ALP-302
Albumin-3.88
A/G-2.94
CUE
Albumin+
Sugar-nil
Pus cells-3-4
Epithelial cells-2-3
Dengue NS1-negative
Smear for malaria parasite-negative
31/7/23
RFT
Urea-28
Creatine - 1.7
Na+ -130
K+ - 3.1
Cl- 100
Hemogram
Hb-9.2
TLC-14,300
MCV-76.9
MCH-28.0
RBC-3.17
Platelet-2.3
Spot urine protein- 12
spot urine creatine- 23.3
urine protein/creatine ratio-0.51
Hemogram on 1/8/23
Hb-13.5
TLC-8,500
MCV-75.9
MCH-27.1
Platelet-2.09
CUE on 1/8/23
Albumin-trace
Sugar-nil
Pus cells-1-2
Epithelial cells-2-3
Blood cells-6-7
Provisional diagnosis
Pyrexia under evaluation?cystitis,AKI with denovo DM2
Treatment
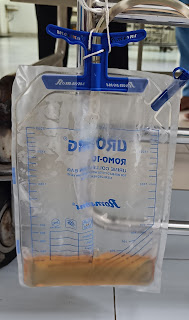
1).i.v NS 50ml/hr
2)inj.PAN 40mg i.v/od
3)inj.MONOCEF 1gm iv/bd
4)inj.LASIX 20mg iv/bd
5)syp.CITRALKA po/tid(10ml)
6)syp.CREMAFIN po/bd
7)inj.HAI sc/tid according to blood glucose levels
8)grbs-7hr profile
9)Tab.DOLO650 mg Po/tid









Comments
Post a Comment